Result
How We Helped a National Insurance Provider Identify $4.2M in Fraud—And Cut Investigation Time by 68%
Client Overview
Goal
Problem
▫️ Fraudulent claims were slipping through due to siloed systems and limited historical analysis
▫️ Investigators spent weeks manually reviewing low-risk claims
▫️ Patterns of coordinated fraud were rarely surfaced until after payouts
▫️ False positives created unnecessary costs and legal headaches
Solution
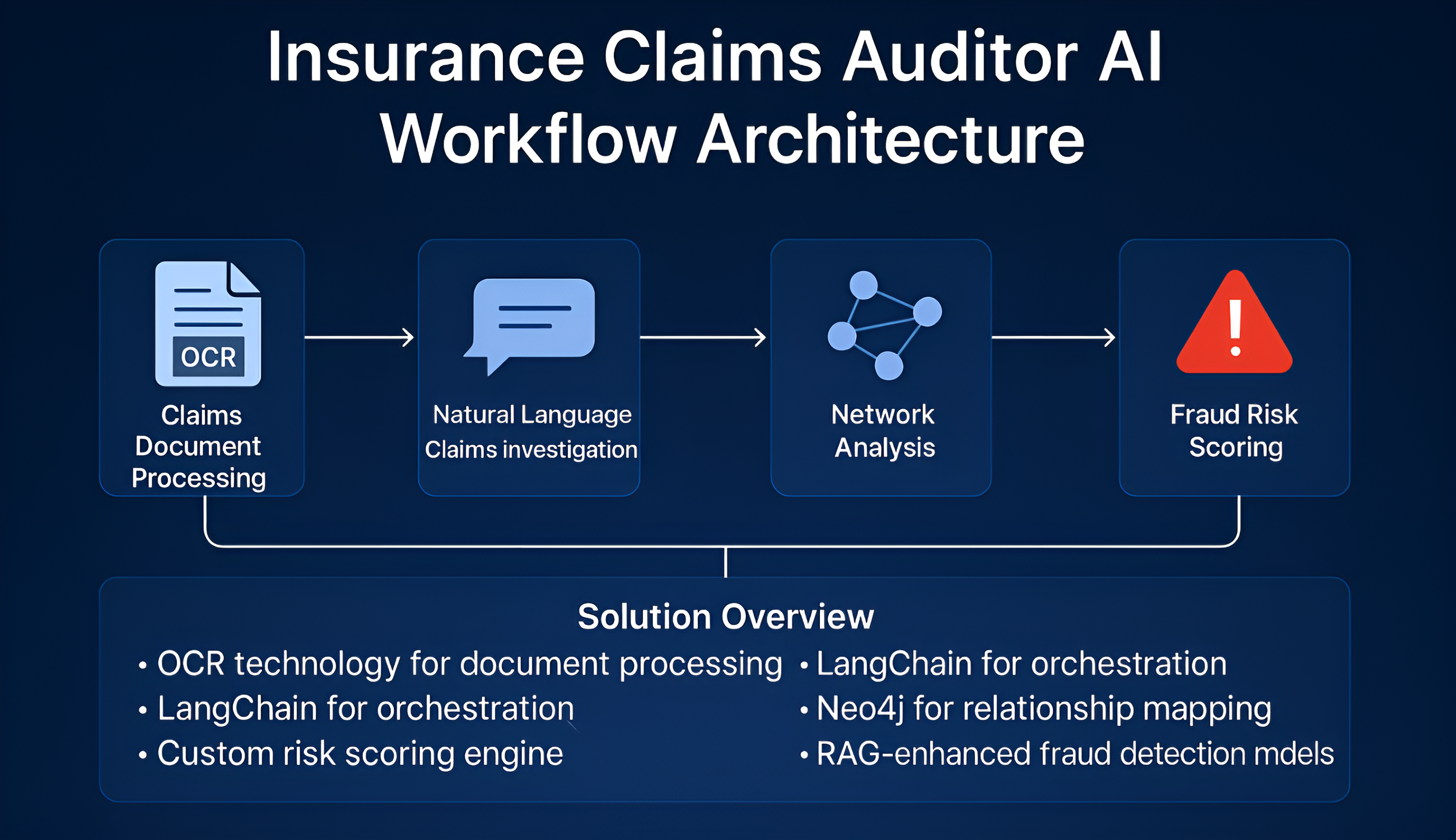
TechSteck Solutions built an AI-powered Claims Auditor—an advanced RAG-based fraud detection system that parses documents, analyzes relationships, and flags risk with source-cited explanations. It combines OCR, graph analysis, and machine learning to spot fraud faster and smarter
▫️ OCR engine for document digitization and structured extraction
▫️ LangChain for orchestration and natural language interface
▫️ Neo4j for graph-based network analysis
▫️ Custom fraud risk engine with ML-based scoring
▫️ GPT-powered RAG models for real-time question answering
How It Works
Conclusion
By combining OCR, network analysis, and advanced risk scoring, TechSteck Solutions gave this insurer a proactive fraud detection system that improves over time, surfaces previously invisible risks, and slashes wasted time on low-risk claims—turning compliance into a competitive advantage.
Contact Us
©2025 | Techststeck Solutions